When patients cannot afford their medications, they may rely on financial assistance from pharmaceutical manufacturers and other third parties to meet their health plan’s cost-sharing responsibilities and fill their prescriptions. The value of this financial assistance typically counts toward the health plan’s deductible or maximum out-of-pocket limit, unless the health plan has implemented a copay accumulator program. Copay accumulator programs exclude the value of financial assistance from third parties from counting toward the health plan’s deductible or maximum out-of-pocket limit. These programs may force patients to switch or stop taking their treatment because they cannot afford their out-of-pocket costs once their financial assistance has been exhausted. Copay accumulator programs may disproportionately affect patients whose conditions are managed or treated by drugs in specialty formulary tiers that require greater cost-sharing from the patient.
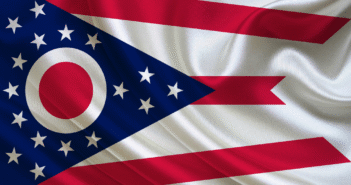
States have begun to introduce legislation to address copay accumulators. Please click on the map below for information about legislation introduced this session.
Last Updated on May 11, 2019 by Aimed Alliance